Medical Biller Support That Protects Your Revenue Cycle
Get billing support that keeps your revenue flowing. MedVirtual’s Virtual Medical Billers handle claims processing, payment posting, and A/R follow-ups with precise, compliant workflows, so you cut denials, speed reimbursements, and maximize every dollar earned.
Starting at $11/hour
Trusted by 250+ Healthcare Practices Across the US
Why Reliable Medical Billing Support Increases Revenue and Reduces Risk
Dental practices thrive when clinical coordination runs smoothly. Our licensed, HIPAA-trained Virtual Dental Nurses provide essential support, managing treatment records, patient follow-ups, and chart accuracy, so your in-office staff can focus on hands-on care and patient relationships.


What a Virtual Medical Biller Can Do for Your Practice
Review superbills for coding accuracy
Create & submit clean claims
Verify payer eligibility & coverage
Track claims to ensure acceptance
Post EOBs, EFTs & remittances
Reconcile payments with payer schedules
Manage patient balances & adjustments
Flag discrepancies for resolution
Track unpaid or underpaid claims
Contact payers for status & resolution
Submit appeals for denied claims
Maintain detailed follow-up logs
Verify insurance before appointments
Record copays, deductibles & coverage
Communicate benefits to front desk/billing
Prevent patient eligibility issues



How MedVirtual Delivers Expert, Compliant Billing Support
Every MedVirtual Medical Biller completes 200+ hours of training through our Healthcare Operations Academy, including payer guidelines, EOB management, and HIPAA compliance — all designed by certified U.S. billing experts.
Each candidate passes billing accuracy assessments, HIPAA certification, and system proficiency tests in platforms like Kareo, AthenaCollector, AdvancedMD, eClinicalWorks, and DrChrono.
Our QA and account management teams monitor accuracy, turnaround times, and collection KPIs, ensuring consistent performance and accountability.
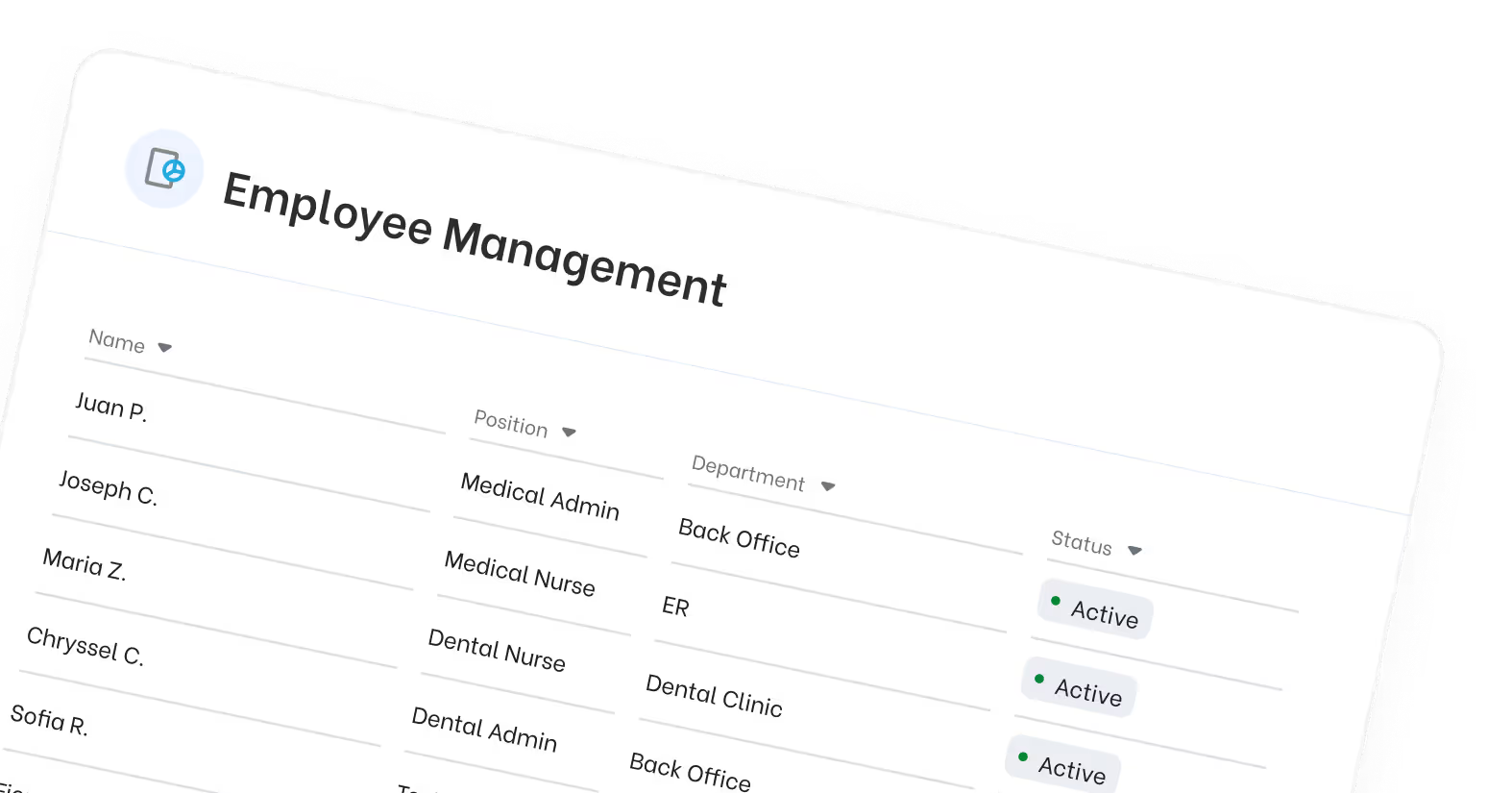
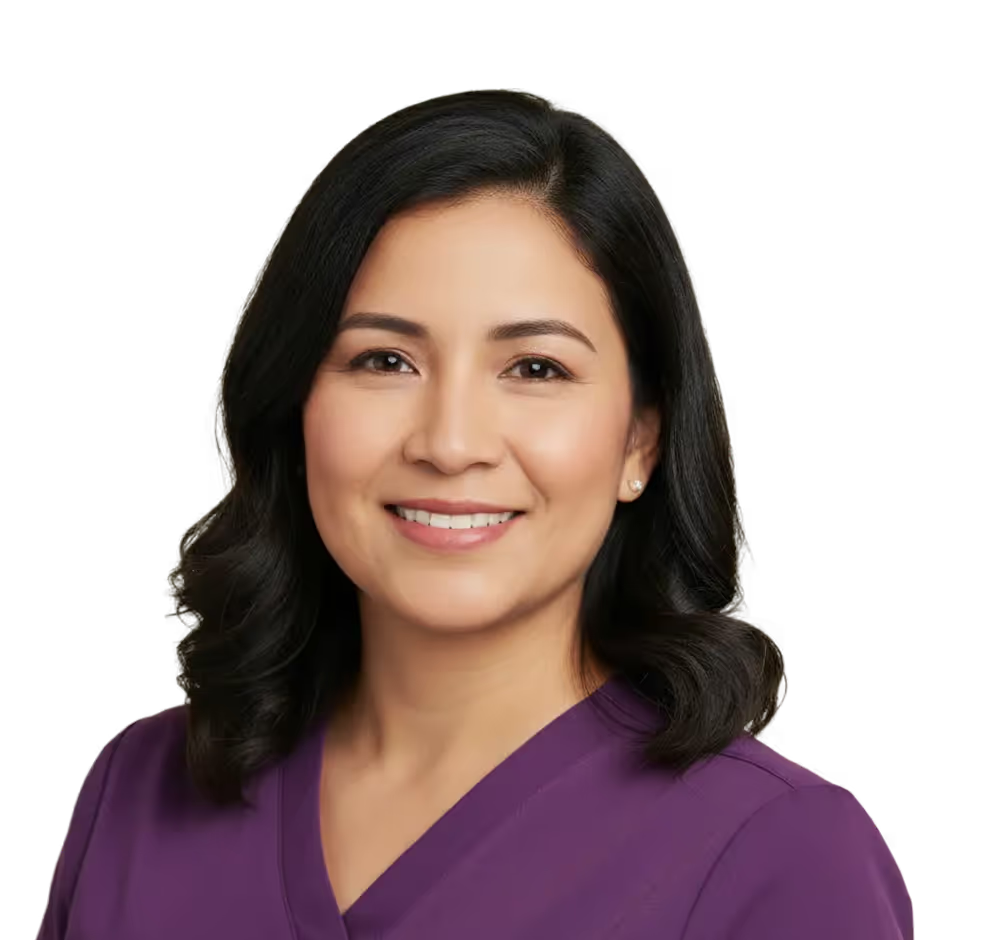
Meet Our Carefully Screened Professionals


Gina excels in processing medical claims, resolving billing issues, and ensuring accurate financial records. She is passionate about advocating for patients' rights and optimizing revenue cycle management.



Jeffrey has a robust background in urgent care settings, adept at patient triage and immediate care protocols. She has successfully handled high-pressure situations and is trained in emergency response techniques.



Diane excels in patient account management, claims processing, and revenue cycle optimization. She is committed to delivering quality service and ensuring compliance with healthcare regulations.
Our Impact in Numbers
The Smarter, More Affordable Way to Staff Your Practice
Medical Billing Expertise Across Specialties
Our Virtual Medical Billers understand the unique workflows and payer nuances of your specialty
Procedure bundling
diagnostic coding
payer pre-authorization tracking
Post-surgical billing
workers’ compensation claims
documentation review
Preventive-care coding
modifier management
recurring claims
Couldn’t find your specialty?
We’ll match you with a Medical Biller experienced in your payer mix and documentation requirements.
Trusted by Practices That Put Patients First
Our clients don’t just hire virtual staff; they continue to partner with us because of the results. Healthcare providers share their experience working with virtual medical assistants from MedVirtual.











It’s Easy to Start
Share your billing systems and payer workflow.

Interview HIPAA-trained, system-proficient billers.
We handle onboarding, secure access, and reporting setup.
Your Guide To Common Questions & Solutions
A MedVirtual Medical Biller manages claim creation, submission, follow-up, and payment posting, ensuring your revenue cycle runs smoothly. They work remotely inside your EHR and clearinghouse, fully HIPAA-compliant and transparent.
Yes. Every Medical Biller completes HIPAA training and certification through our Healthcare Operations Academy, covering PHI security, claims workflows, and payer communication protocols.
Absolutely. Our billers are experienced in major billing systems, including Kareo, AdvancedMD, AthenaCollector, DrChrono, and eClinicalWorks. We configure secure access during onboarding.
Through a structured QA process: random claim audits, double-verification for coding, and ongoing accuracy tracking. We maintain >98% first-pass acceptance rates for most clients.
We providMulti-provider clinics, family medicine, and specialty practices with moderate-to-high claim volumes, or any practice struggling with delayed reimbursements or denied claims.e ongoing QA, HIPAA audits, and clinical documentation reviews. Each nurse’s performance is tracked monthly, with regular retraining and reporting to maintain 97% satisfaction and accuracy rates.
All billing operations follow HIPAA and payer regulations. Billers use encrypted systems, access logs, and operate under signed Business Associate Agreements (BAAs) to ensure legal and data compliance.