Virtual Medical Staff for Healthcare Practices: When Remote Teams Make Sense

In 2026, healthcare practices are no longer limited to traditional, in-office staffing models. Advances in technology, shifting patient expectations, and ongoing workforce shortages have made virtual medical staff a practical and reliable option for many organizations.
What was once viewed as a temporary solution or backup plan has now become a core part of day-to-day operations for modern healthcare practices. From administrative support to clinical documentation, remote teams are helping practices stay efficient without compromising patient care.
Still, virtual staffing isn’t a one-size-fits-all solution. The real question is not whether remote teams work, but when they make the most sense for your practice.
At MedVirtual, we’ve seen how thoughtfully integrated virtual medical staff can reduce operational strain, improve workflows, and support sustainable growth. Below, we explore the situations where remote teams deliver the most value in today’s healthcare environment.
When Remote Teams Make Sense: Identifying Operational Pain Points
Transitioning to virtual medical staff is most effective when it addresses clear, day-to-day challenges. Rather than replacing in-office teams, remote professionals are best used to relieve pressure points that slow operations or affect patient experience.
Healthcare practices often find that virtual teams make the most sense in the following situations:
1. High Administrative Workload
When front-desk and administrative staff are spending most of their day handling phone calls, insurance verification, scheduling, and billing tasks, patient-facing work can suffer. Virtual medical staff help absorb these responsibilities, allowing in-office teams to stay focused on patient care.
2. Rapid Practice Growth
As practices expand, staffing needs increase quickly. Physical space, equipment, and onboarding timelines can make in-office hiring difficult. Remote teams allow practices to scale administrative support without the constraints of office capacity or renovation costs.
3. Telemedicine and Geographic Expansion
For practices offering telehealth services or serving patients across multiple locations, remote coordinators act as a consistent point of contact. They manage digital intake, appointment coordination, and basic technical support, helping providers focus on clinical interactions.
4. Budget and Cost Pressures
Staffing and overhead remain two of the largest expenses for healthcare organizations. Virtual medical staff can reduce costs related to office space, equipment, and local labor, while still providing experienced administrative and clinical support.
5. Extended Coverage Needs
Patient questions and administrative requests don’t always fit within standard office hours. Virtual teams make it possible to offer extended or after-hours support without requiring in-house staff to work longer shifts.
Team Dynamics: Integrating Virtual Staff into Your Practice
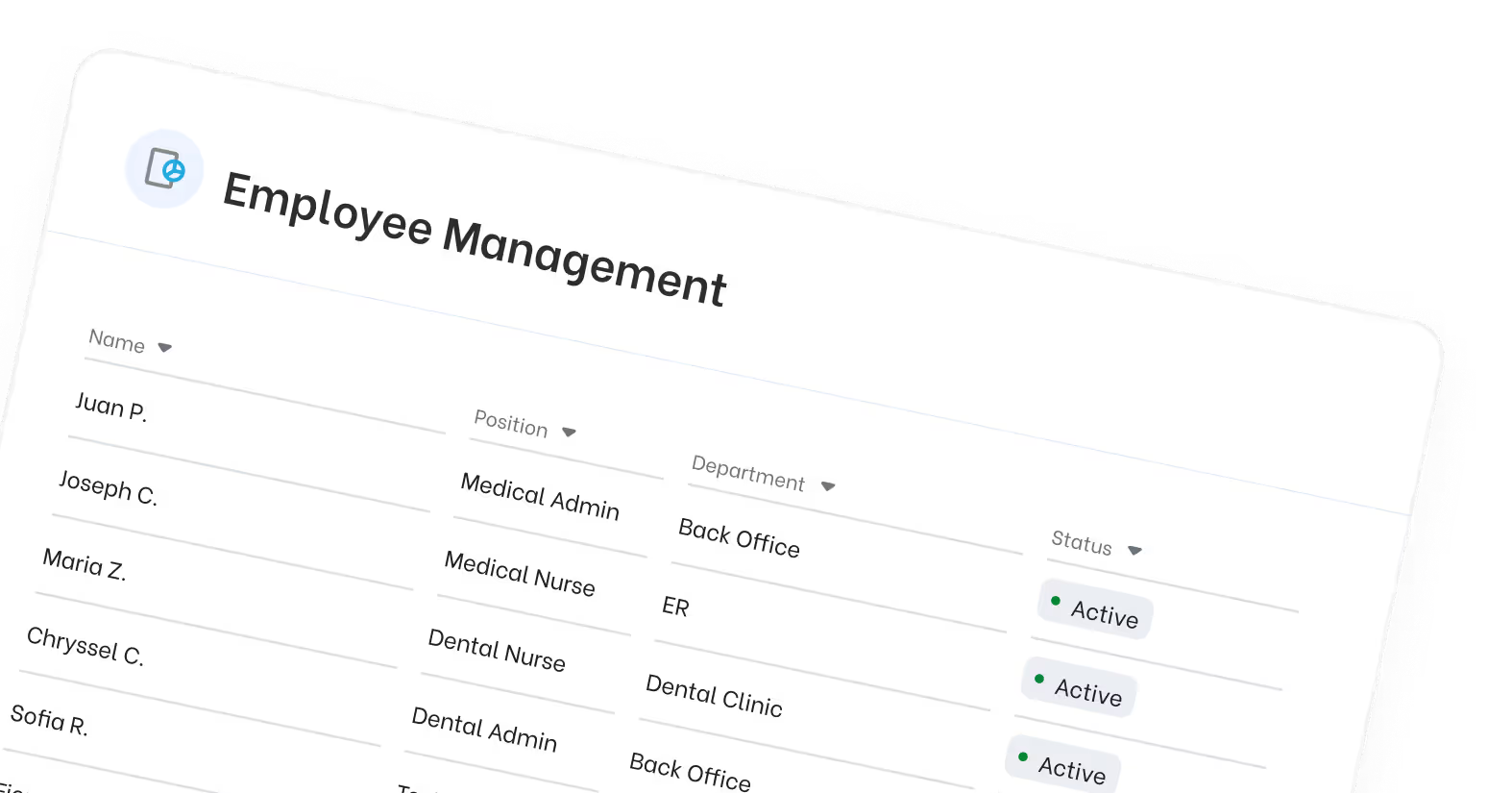
Integrating virtual staff into a healthcare practice allows healthcare organizations to access a global pool of experienced administrative professionals, helping overcome local staffing shortages that continue to challenge the healthcare industry. This approach supports modern healthcare delivery without relying solely on traditional in-office hiring models.
Clear communication is essential when working with remote professionals. Establishing multiple communication channels and training teams in communication best practices helps virtual assistants and in-house staff stay aligned, reducing errors and improving collaboration across the healthcare team.
A structured onboarding process ensures virtual staff understand internal systems, workflows, and compliance requirements. Healthcare providers should support remote work with secure technology infrastructure, including encrypted communication platforms and VPN access, while conducting regular audits to maintain regulatory standards and protect patient data.
Building a cohesive team culture is equally important. Including virtual assistants in routine meetings helps maintain morale and ensures consistency in patient care, even when teams are distributed across different locations and time zones.
Recent regulatory changes have further supported remote collaboration. As of 2026, CMS has established permanent virtual supervision of clinical teams via audio-video technology, and new CPT codes now allow shorter remote interactions to be reimbursable, making virtual staffing more practical for healthcare practices.
Key Healthcare Virtual Assistant Roles Shaping 2026 Healthcare
Healthcare virtual assistants in 2026 are no longer generalists. Many practices now rely on specialized virtual staff to reduce administrative burden and support patient care more efficiently across healthcare settings.
Medical Virtual Assistants (VMAs) support day-to-day administrative tasks such as managing patient records, data entry, scheduling, patient intake, and patient follow-ups. In 2026, hiring a full-time VMA can cost under $2,000 per month, compared to roughly $6,000 for local in-person staff, creating meaningful cost savings for healthcare organizations.
Virtual Medical Scribes assist medical professionals by managing documentation during video calls, helping reduce administrative load and allowing healthcare professionals to focus on clinical expertise rather than note-taking.
Virtual Nurses provide telehealth support, assist with technical issues, and help manage chronic conditions using data from wearable devices. They also support patient inquiries, triage urgent issues, and improve service delivery through flexible support across time zones.
Remote Patient Monitoring (RPM) Specialists track patient data from connected devices and flag significant changes for healthcare providers, supporting continuous care while improving operational efficiency.
Revenue Cycle and Billing Support Staff assist with insurance verification, billing questions, and claims support, helping healthcare systems address administrative tasks that consume nearly 25% of total healthcare spending in the United States.
The Strategic Edge: Beyond Just “Extra Help”
The traditional hiring model in healthcare is not scaling with the demands of modern healthcare delivery. Staffing shortages, rising administrative costs, and increasing compliance requirements make it difficult for most practices to rely solely on an in-house team.
Virtual staffing solutions allow healthcare organizations to access a global pool of experienced administrative professionals, many with strong medical terminology knowledge and HIPAA compliance training. This breaks geographic barriers and reduces dependence on commuting distance or limited local talent pools.
Employing virtual medical staff can reduce overhead costs by up to 60–70% by eliminating expenses tied to office space, furniture, IT equipment, payroll taxes, and employee benefits. Many practices also save up to $11,000 per year per remote worker while maintaining quality control and team performance.
Virtual assistants allow healthcare organizations to scale operations up or down with minimal financial impact. This flexibility is especially valuable during seasonal demand spikes or strategic labor shortages, where remote teams can fill gaps without the high costs of traditional locum contracts.
In addition, 24/7 availability improves patient satisfaction by handling patient inquiries, appointment requests, and follow-ups outside standard business hours—without increasing administrative load on medical practices.

Is Your Practice Ready to Evolve?
In 2026, regulatory changes have made virtual healthcare operations more viable than ever. New CPT codes now support reimbursable remote team interactions, and CMS has established permanent virtual supervision of clinical teams through audio-video technology.
For many healthcare organizations, the key difference is no longer if virtual staff fit—but how they are integrated. Practices that focus on effective communication, compliance, and structured team integration are reducing administrative burden while maintaining high standards of patient care.
Rather than replacing the in-house team, most practices are adopting a hybrid approach—using virtual support to improve operational efficiency, patient satisfaction, and long-term resilience.