CPT Code 90471: Billing, Documentation & Reimbursement Guide
The healthcare system in the United States relies on accurate medical coding to link billing and reimbursement with proper medical record maintenance. Incorrect coding often leads to denied claims, causing regulatory and financial issues. A CPT code is a standardized code U.S. healthcare providers use to describe medical, surgical, and diagnostic services for billing and documentation. This system ensures clear communication among physicians, insurers, and patients.
CPT Code 90471 specifies the administration of immunizations via injection. Proper use by physicians, hospitals, clinics, and other providers is essential to meet U.S. payer requirements, including Medicare, Medicaid, and private insurers, and to comply with federal submission standards. This guide covers CPT Code 90471’s definition, application, billing and documentation standards, reimbursement policies, and common errors.
Healthcare professionals in the U.S. will gain a clear understanding of CPT Code 90471 to ensure accurate billing, reduce claim denials, and optimize reimbursement under the American healthcare system.
What is CPT Code 90471?
Current Procedural Terminology (CPT) code 90471 is maintained by the American Medical Association (AMA) and is a fundamental component of the U.S. medical billing system. This code is specifically used for billing the administration of a single vaccine injection to a patient. It does not include the cost of the vaccine product itself. CPT 90471 applies only to the first vaccine given by injection during a patient’s visit. Accurate documentation and proper coding are essential to facilitate smooth billing processes, reduce claim denials, and ensure compliance with U.S. payer regulations, including Medicare, Medicaid, and private insurance providers.
Key Features of CPT Code 90471
- Applies to all percutaneous, intradermal, subcutaneous, intramuscular, and other injectable vaccines administered within the United States.
- Used for vaccine administration across all patient age groups, including pediatric and adult populations.
- Exclusively for the first vaccine injection given during a patient’s visit.
- Each additional vaccine administered during the same encounter must be billed separately using CPT Code 90472.
- Standard coding practice in U.S. healthcare settings including physician offices, hospitals, urgent care centers, and community health clinics.
- Covers only the administration service; the vaccine product itself requires a distinct CPT code for billing purposes.
- Ensures compliance with U.S. payer policies, including Medicare, Medicaid, and private insurers.
- Helps providers secure appropriate reimbursement and avoid claim denials.
When to Use CPT Code 90471?
Healthcare providers should apply CPT Code 90471 whenever they give patients a single vaccine dose through an injection treatment at their typical appointment. The code excludes both simultaneous vaccine administration and injectable vaccine procedures.
Example Scenarios
- An annual intramuscular flu shot service performed by pediatricians qualifies for CPT 90471.
- The medical facility provides patients receiving treatment for wound injuries with tetanus vaccine treatments through CPT 90471.
- The administration of a hepatitis A vaccine at a travel clinic should be coded under CPT 90471.
- The provider performs a single-dose pneumonia vaccination under CPT 90471.
- In urgent care, the accident victim receives a rabies vaccine from a nurse who performs CPT 90471.
When NOT to Use CPT Code 90471
- The use of CPT 90471 describes the billing for the initial vaccine, yet each subsequent vaccine administered at the same appointment needs CPT 90472.
- The use of CPT Code 90473 becomes appropriate when the vaccine is introduced through oral or nasal routes.
CPT Code 90471 vs. 90472: Understanding the Difference
Medical billing confusion occurs when healthcare providers must differentiate between CPT 90471 and CPT 90472.
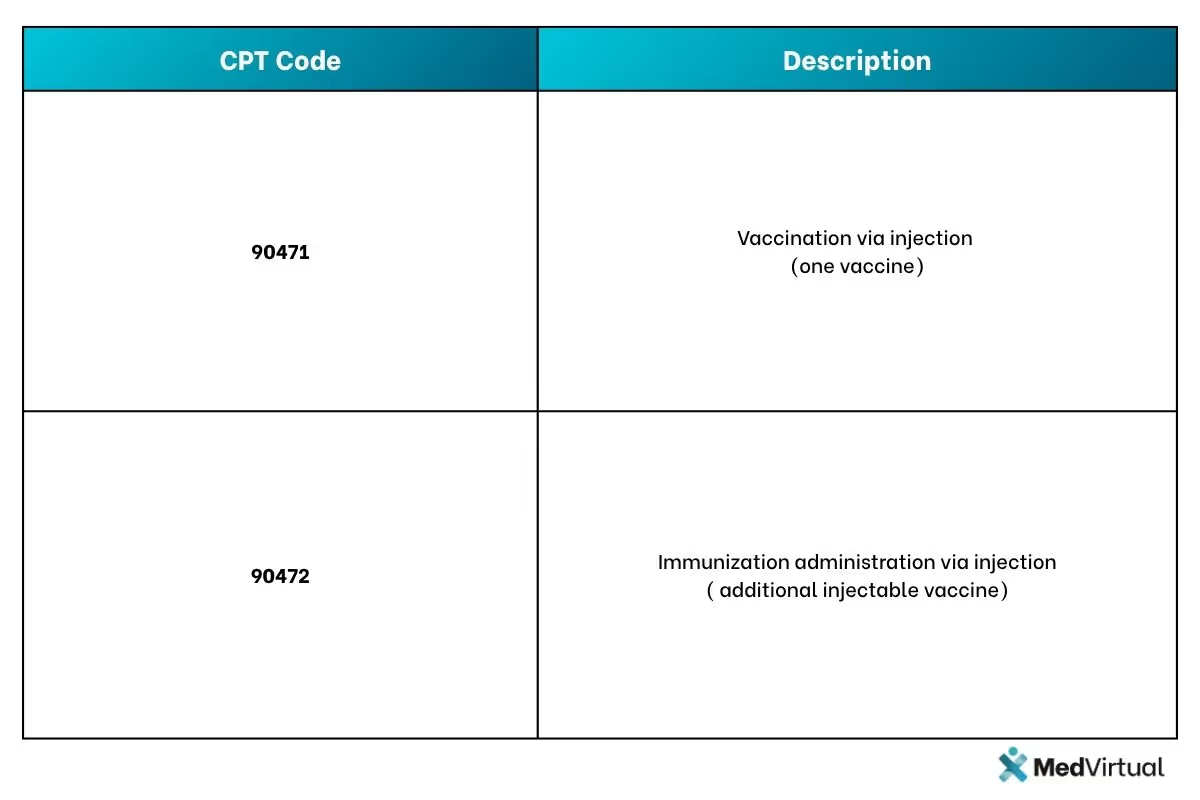
Key Takeaways
The provider should bill CPT 90471 when administering an initial vaccine through injection. Medical staff should use CPT 90472 to bill the administration of additional vaccines when more than one vaccine occurs in a single office visit. The medical provider must submit CPT 90471 for the initial vaccine, followed by CPT 90472 for every additional vaccine provided during the same appointment. The administration of oral and intranasal vaccines should be billed with the CPT Code 90473.
Example of Multiple Vaccines Given During a Visit
The clinic provides standard vaccinations to the patient, which include two procedures:
- An influenza vaccine (intramuscular injection) → Billed as CPT 90471.
- A tetanus-diphtheria booster (Td) vaccine (subcutaneous injection) → Billed as CPT 90472.
The clinic receives full reimbursement by correctly billing each vaccine with CPT 90471 for the first dose and 90472 for each subsequent vaccine.
CPT Code 90471 vs. 90473: Injectable vs. Oral/Nasal Vaccines
The coding difference between injectable vaccines CPT 90471 and oral or intranasal vaccines CPT 90473 needs to be recognized.
Example Scenarios
- A pediatrician provides an intramuscular flu shot, which qualifies for CPT 90471.
- The pharmacist delivers FluMist through the nasal route, which justifies billing with CPT 90473.
To provide vaccine services to patients who need both injection and nasal vaccine during one visit, physicians should use CPT 90471 for injections and CPT 90473 for intranasal treatment.
Insurance Coverage, Modifiers, and Common Billing Errors for CPT 90471
It takes more than just using the correct code to get paid for CPT 90471. You also need to understand how insurance covers it, when to use modifiers, and how to avoid typical billing errors. To assist you in filing clean claims and receiving reimbursement without any problems, we'll go down the insurance criteria, modifier regulations, and billing issues below.
Insurance and Payer Guidelines
Medicare and Medicaid public health insurance provide vaccine administration coverage, yet payment procedures differ between states. Private insurance plans contain immunization administration under their preventive care benefits. While employer health plans through wellness programs provide total coverage of vaccinations to their members.
Modifiers for CPT 90471
The application of modifiers helps identify particular situations for billing CPT 90471 appropriately.
- The billing modifier 25 should be used when both an evaluation and management service and immunization service are performed on the same day.
- The use of Modifier 59 is required when the patient needs two doses of the same vaccine administered in distinct locations, such as different arm areas.
Common Billing Errors and How to Avoid Them
- The coding standard for CPT 90471 applies to the first vaccine only during a single visit; therefore, additional vaccines must be processed through CPT 90472.
- Failure to mention vaccine details warrants documentation of the manufacturer's name, lot number, and expiration date.
- A vaccine must be connected with Z23 (Encounter for immunization) as the proper ICD-10 diagnosis code.
ICD-10 Codes Commonly Used with CPT 90471
Importance of ICD-10 Codes in U.S. Billing
For successful processing of CPT Code 90471 claims within the United States healthcare system, it is essential that providers pair vaccine administration with the correct ICD-10 diagnosis codes. Incorrect or missing diagnosis codes can lead to claim denials by U.S. insurers, including Medicare, Medicaid, and private payers. The most commonly used ICD-10 code for CPT 90471 in the U.S. is Z23 (Encounter for Immunization).
Additional Relevant ICD-10 Codes
In certain cases, additional ICD-10 codes are required to support claims involving CPT 90471, particularly for vaccines administered as part of post-exposure prophylaxis or specific medical conditions. Examples of these codes used in U.S. billing include:

While Z23 is sufficient for routine immunizations, U.S. healthcare providers must include these additional diagnosis codes when billing for vaccines related to specific injury exposures or medical conditions to ensure compliance with payer requirements and avoid claim denials.
Documentation Requirements for CPT 90471
Why Proper Documentation is Essential
Accurate documentation is required to process CPT 90471 claims successfully. Proper documentation linked to ICD-10 code Z23 (Encounter for Immunization) ensures full reimbursement, prevents claim denials, and supports compliance with Medicare, Medicaid, and private payer audits. It serves as legal proof of vaccine administration and maintains continuity of care.
Common claim denials result from incomplete documentation, such as missing vaccine manufacturer, lot number, expiration date, or administration site, which can delay or reduce reimbursement. Thorough vaccine records also protect providers in case of adverse reactions or disputes.
Essential Documentation Elements
To meet U.S. payer requirements, records must include:
- Vaccine Details: Manufacturer, lot number, expiration date, and dosage amount to track vaccine safety and recalls.
- Administration Route and Site: Specify injection method (intramuscular, subcutaneous, intradermal) and exact site (e.g., left deltoid). Example:
“Physician injected 0.5mL intramuscularly into the left deltoid using a 23-gauge needle.” - Patient Identification and Consent: Accurate patient name, age, medical record number, and documented informed consent prior to vaccination.
- ICD-10 Diagnosis Code: Use Z23 for routine immunizations. Add specific codes when vaccinating for post-exposure prophylaxis (e.g., rabies).
- Provider Identification: Signature or electronic authentication of the administering healthcare professional.
- Observation of Adverse Reactions: Document any immediate side effects or note if none observed. Example:
“No immediate adverse reactions observed post-vaccination. The patient tolerated the injection well.”
Missing any of these elements increases the risk of claim rejection or audit delays.
Covid-19 and CPT 90471: Special Considerations
The pandemic emergency caused healthcare providers to encounter distinctive billing scenarios while administering COVID-19 vaccines. Hospitals and health providers continued to invoice for administering free government-provided COVID-19 vaccines at their initial stage.
Billing Covid-19 Vaccine Administration
For example, a patient undergoing their initial Pfizer COVID-19 vaccine dosage at a clinic qualifies for the specific billing procedure.
- 90471- Administration of first COVID-19 vaccine dose.
- 91300- Pfizer Covid-19 vaccine product code (if not provided free by the government)
- ICD-10 Code: Z23- Encounter for Immunization
The administration of a second vaccine dose is billed as 90472 since the initial dose was previously included under 90471:
- 90472- Administration of second dose vaccine (since the first was already billed under 90471)
- 91300- Pfizer Covid-19 vaccine product code
- ICD-10 Code: Z23
A similar correct billing strategy should also be used for boosters to prevent the denial of claims.
The Correct Coding of Covid-19 Vaccinations Matters
The sudden pandemic created awareness about accurate medical coding because it produced essential benefits for both payment distributions and government rule compliance.
Medicare, Medicaid, and other payers need healthcare providers to document vaccine doses correctly while using required billing modifiers for accuracy. Payers conducted frequent audits of insurance claims regarding COVID-19 vaccines as they verified proper billing practices during this period. Healthcare providers became subject to insurer delays when they failed to document vaccine administration procedures correctly.
Maximizing Reimbursement for CPT 90471
Strategies to Ensure Full Reimbursement
The following best practices, when combined, ensure both maximum payments and minimum claim denials:
- Link CPT 90471 to ICD-10 code Z23 during every procedure-related application.
- Independent claims should use CPT 90472 to report additional vaccines given to the same patient during the appointment.
- Outside of the product code report, each vaccine should receive its specific code (for example, the code 90686 represents flu vaccines).
- When you perform an evaluation and management service alongside the vaccines, you must use modifier 25 to avoid payment issues.
- Every payment must include complete details containing the product's lot numbers and manufacturer information.
Reasons for Claims Denials and How to Fix Them
Prudent action toward these medical issues helps enhance claim reimbursement outcomes while minimizing rejections.
Final Overview and Recommendations
CPT code 90471 plays a crucial role in the accurate billing and reimbursement of vaccine administration in the United States. Code 90471 is an essential procedural code dedicated to the initial vaccine given via injection during a patient's office visit. Each additional injectable vaccine administered during the same visit requires billing with CPT code 90472, while oral or nasal vaccine administration should be billed using CPT code 90473. Adhering to correct coding standards helps prevent medical billing errors, ensuring smooth claim processing and timely reimbursement under U.S. healthcare payer policies.
The medical necessity of vaccines is documented through the ICD-10 diagnosis code Z23 (Encounter for Immunization), which must be included with the CPT codes submitted. Additionally, thorough documentation of the vaccine manufacturer, lot number, expiration date, dosage, administration site, and provider signature is critical to meet U.S. payer requirements and comply with medical audit standards.
Following these best coding and documentation practices enables healthcare providers and medical coders across the U.S. to reduce claim denials, maximize reimbursement, and maintain compliance with insurance policies. Efficient medical billing supported by the proper use of CPT code 90471 contributes to the financial stability of healthcare practices and the delivery of quality patient care.
For expert assistance with U.S.-specific medical billing and coding, Reach out to MedVirtual. We specialize in streamlining your billing processes, minimizing claim denials, and maximizing reimbursements within the American healthcare system. Contact us today to ensure compliance and enhance the financial health of your practice.
Frequently Asked Questions (FAQs) about CPT Code 90471
Q1. Can medical personnel use CPT 90471 when providing multiple vaccines in one patient appointment?
No, CPT 90471 is used exclusively for billing the administration of the initial vaccine injection during a patient visit. For each additional vaccine administered during the same appointment, healthcare providers must use CPT 90472. This billing practice is standard across U.S. healthcare settings to ensure proper reimbursement.
Q2. Does CPT 90471 cover the cost of the vaccine itself?
No, CPT 90471 only covers the administration of the vaccine via injection. The vaccine product has its own distinct CPT code, such as 90686 for influenza vaccines or 90715 for Tdap vaccines. Providers must bill separately for the vaccine product and its administration.
Q3. Can CPT 90471 be billed along with an evaluation and management (E/M) office visit?
Yes, CPT 90471 can be billed on the same day as an E/M office visit if the evaluation and management service is significant and separately identifiable from the vaccine administration. In such cases, providers should append modifier 25 to the E/M code to indicate the separate service.
Q4. What is the difference between CPT 90471 and CPT 90473?
CPT 90471 is used for vaccine administration via injection routes, including intramuscular, subcutaneous, and intradermal. CPT 90473 is designated for oral or intranasal vaccine administration, such as the FluMist nasal spray vaccine. Providers must select the correct code based on the vaccine administration route.
Q5. How should pediatric vaccine administration be coded using CPT 90471?
For pediatric patients receiving multiple vaccines during a single visit, providers should bill CPT 90471 for the first vaccine administered via injection. Each additional vaccine requires billing with CPT 90472. Separate CPT codes must be submitted for each vaccine product administered.
Q6. Are there any specific modifiers required when billing CPT 90471 for vaccines administered in different anatomical sites?
Yes, when a patient receives two doses of the same vaccine administered in distinct anatomical locations (for example, left and right arms), modifier 59 should be appended to the second administration code to indicate separate and distinct services to payers.
Q7. What ICD-10 diagnosis codes should be used with CPT 90471 for vaccine administration claims?
The primary ICD-10 code to pair with CPT 90471 is Z23 (Encounter for Immunization). Additional diagnosis codes may be necessary when vaccines are administered for post-exposure prophylaxis or specific medical conditions, such as rabies exposure (e.g., W54.0XXA for dog bite).
Q8. How has the COVID-19 pandemic affected billing practices for CPT 90471 in the U.S.?
During the COVID-19 public health emergency, CPT 90471 was used to bill for the administration of the initial COVID-19 vaccine dose, while subsequent doses used CPT 90472. Providers had to ensure accurate documentation and use appropriate modifiers as required by Medicare, Medicaid, and private payers to receive reimbursement for COVID-19 vaccine administration. Frequent payer audits emphasized the importance of correct coding during this period.