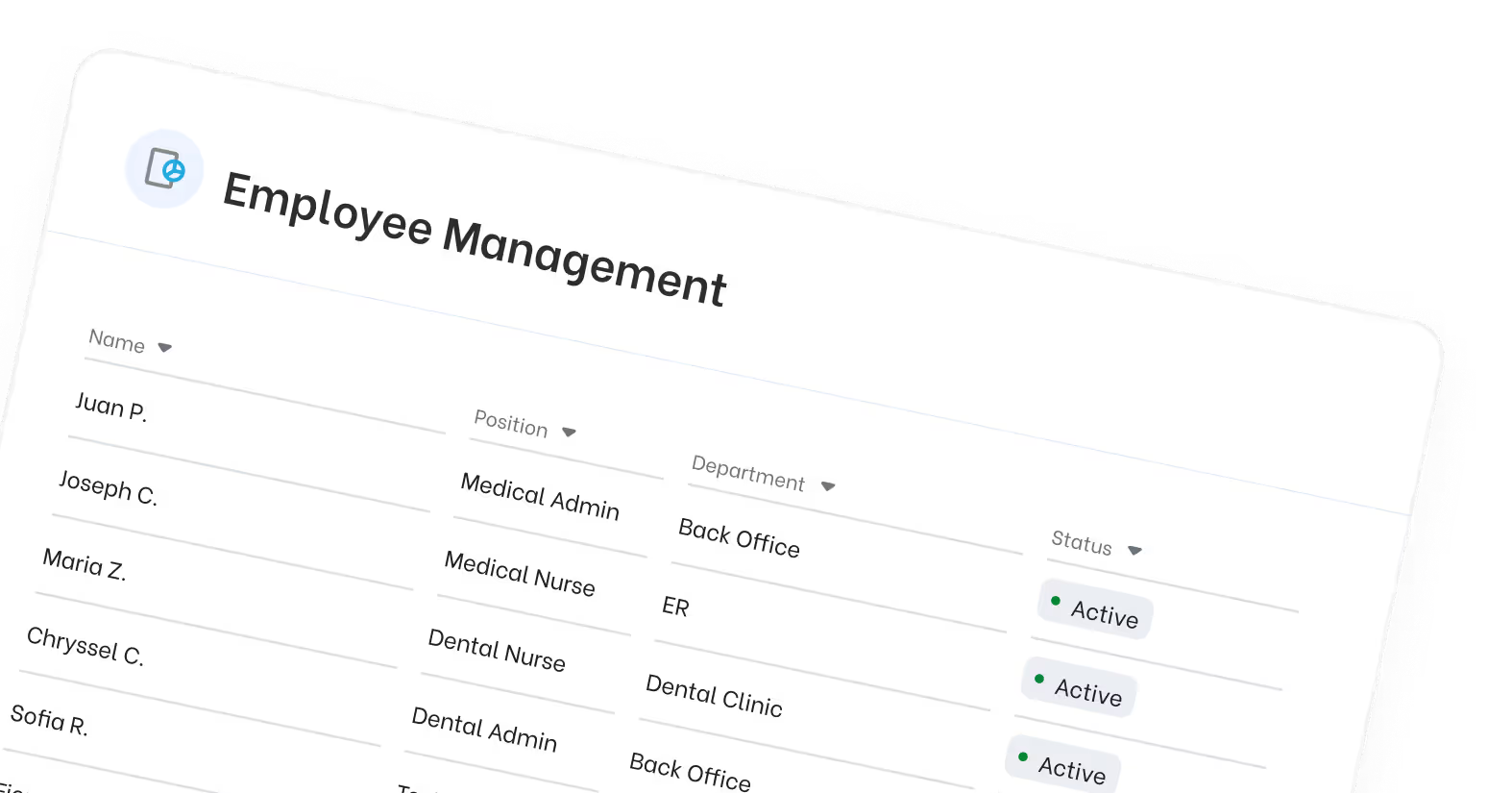
A 2025 Guide to ICD-10-CM Changes in Chronic Pain Management: What You Need to Know
In 2025, a 2025 guide to ICD 10 CM changes in chronic pain management will introduce important updates. This guide will cover essential new codes and modifications, their impact on medical practices, and best practices for accurate documentation.
Key Takeaways for ICD-10-CM Changes in Chronic Pain Management 2025
- Accurate coding with detailed, specific codes is essential to reflect chronic pain type, location, and chronicity.
- Distinguish clearly between acute and chronic pain, documenting the time frame defining chronic pain in provider notes.
- Use appropriate postoperative pain codes only for pain linked to specific complications, not for expected postoperative pain immediately after surgery.
- Combine site-specific pain codes with general pain codes when needed to fully describe the patient’s condition.
- Avoid unspecified pain codes when more detailed documentation is available to ensure accurate coding and reimbursement.
Why Accurate ICD-10 Coding for Chronic Pain Matters in 2025
Accurate use of ICD-10-CM diagnosis codes for chronic pain is essential for healthcare professionals in 2025. As the scope of pain disorders expands, including chronic postprocedural pain, pain due to trauma, and pain not elsewhere classified, documentation must reflect the nature, location, and underlying etiology of the patient’s condition. Proper coding is not just a billing requirement but foundational for effective pain management, care coordination, and long-term patient outcomes.
With the continued evolution of ICD-10 standards, practitioners must consider the role of psychological factors, underlying conditions, and site-specific attributes when assigning diagnosis codes. Conditions like chronic pain syndrome, complex regional pain syndrome, and central pain syndrome now require increased specificity, down to whether pain is unilateral or bilateral, linked to the nervous system, or categorized as localized pain of unspecified type.
Key Considerations for 2025 ICD-10 Pain Coding:
- Chronic pain is often a primary diagnosis, especially when it persists beyond the initial injury or is no longer attributable to the underlying condition.
- New and refined ICD-10 codes address both acute and chronic forms, including distinctions between acute post-thoracotomy pain and chronic post-thoracotomy pain.
- Coders must differentiate between pain due to external causes, pain from prosthetic devices, and neoplasm related pain, whether acute or chronic.
- The inclusion of psychological factors associated with pain, such as anxiety, depression, or cognitive impairment, adds new layers to code assignment and reimbursement.
Proper ICD-10 coding also ensures that conditions such as pain disorders exclusively related to psychological factors, pelvic and perineal pain, or lumbosacral region symptoms are classified correctly and in alignment with payer requirements. These updates directly impact how physicians document pain control strategies, assess patient risk, and select treatment modalities based on the diseases of the nervous system.
In 2025, using the correct billable specific code instead of a billable non-specific code can determine whether your claim is reimbursed or rejected. Clinical documentation must now include more detail, such as laterality, chronicity, and associated behavioral signs, to remain compliant and clinically relevant.
By aligning pain-related diagnoses with current ICD-10-CM guidelines, healthcare providers can reduce denials, improve patient outcomes, and strengthen the integrity of their chronic pain management programs.
Chronic Pain Definitions Refresher
For ICD-10-CM coding, acute pain is defined as pain lasting less than three months, typically linked to a specific external cause such as trauma or surgery, and should be coded with detailed site and laterality information.
Chronic pain, lasting three months or longer and often persisting beyond the initial injury or underlying cause, is treated as a primary diagnosis with specific codes reflecting its chronicity and etiology, including chronic pain syndrome, chronic postprocedural pain, and neoplasm-related pain.
Accurate coding depends on provider documentation clearly stating pain duration and chronicity to guide assignment of appropriate billable specific codes like G89.21, G89.28, G89.29, or G89.4, ensuring claims reflect the true clinical status and support effective chronic pain management.
2025 ICD-10-CM Coding Updates Snapshot
The 2025 updates to ICD-10-CM diagnosis codes include enhanced detail for a range of chronic pain conditions, allowing providers to code more precisely for pain disorders, their underlying causes, and associated psychological factors. This improved specificity is critical for reimbursement accuracy, treatment planning, and compliant documentation in chronic pain management.
Updates affect how providers must code:
- Chronic pain due to trauma
- Chronic postprocedural pain
- Pain not elsewhere classified
- Complex regional pain syndrome
- Neoplasm related pain acute or chronic
- Pain conditions with related psychological factors associated
Below is a practical reference of key ICD-10-CM codes for 2025, grouped by diagnostic focus:
.avif)
These codes should be used as the primary diagnosis when pain is the main reason for the encounter, particularly when the underlying cause is no longer present or clearly established.
Site-Specific and Neurological Pain Codes

These codes are commonly added to represent nervous system involvement, limb pain, or diseases affecting pain perception or nerve conduction.
Behavioral and Psychological Factors Affecting Pain

For patients with related psychological factors, such as chronic pain affecting mood, cognition, or behavior, these codes should be documented to reflect the biopsychosocial impact of long-term pain.
Special Categories and Common Complications

These codes cover chronic pain not elsewhere classified, complications from implants, and localized pain unspecified type that may not have an easily identifiable cause.
Key 2025 ICD-10 Coding Notes:
- Use billable specific codes where possible to avoid claim denials.
- Combine G89 series codes with site-specific or nerve-related codes when applicable.
- Document if the pain is acute, chronic, or related to psychological factors.
- Do not code generalized pain NOS when more specific documentation is available.
By incorporating the correct type code to pain, whether it's chronic post thoracotomy pain, pain related to neoplasms, or pain disorders with psychiatric overlay, providers ensure accurate claim reporting and a more comprehensive reflection of the patient’s condition.
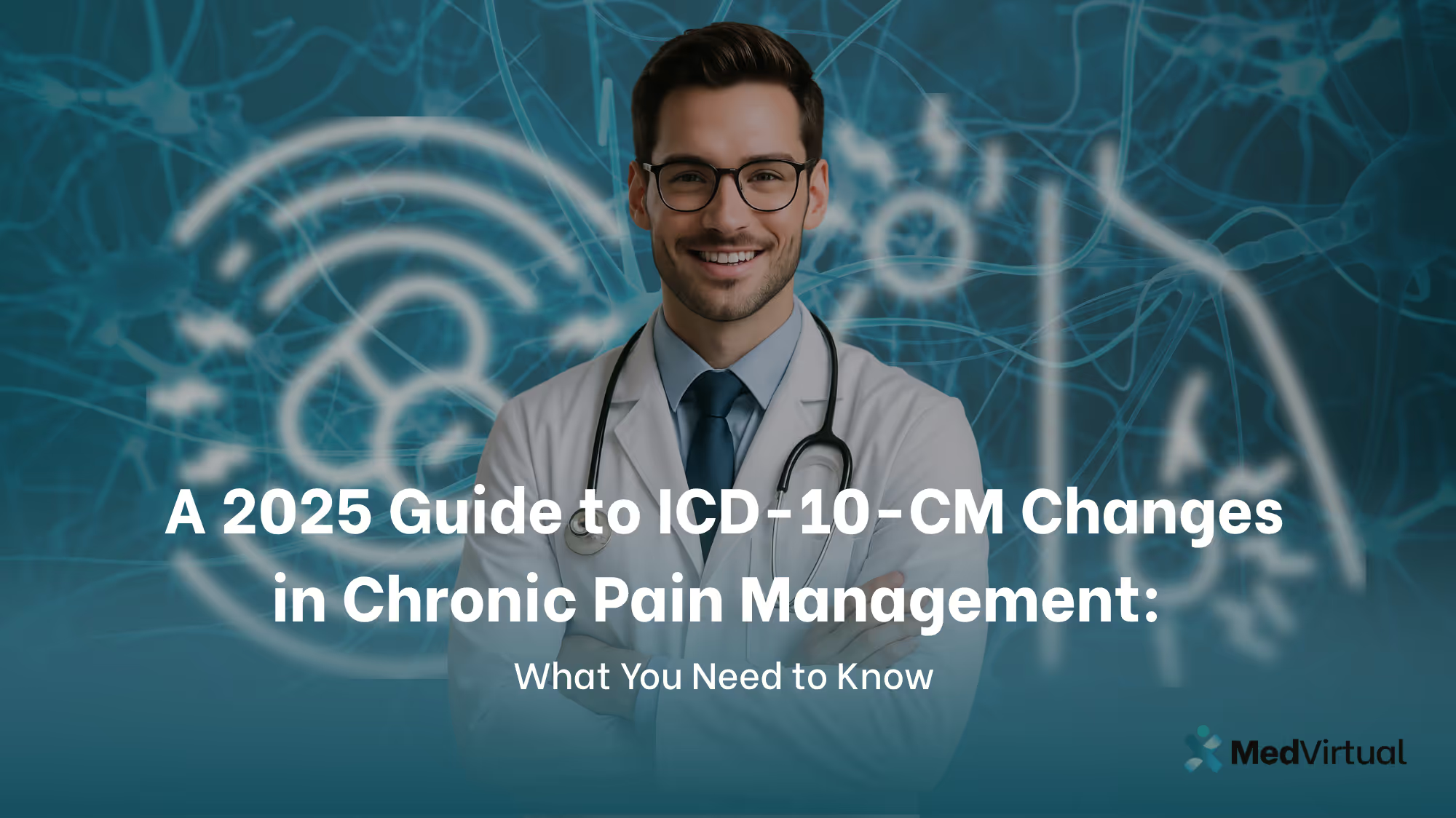
Site-Specific Pain Coding Cheat Sheet
Effective pain documentation and coding require more than just identifying that a patient is in pain, it demands precision by site, laterality, and pain type. The ICD-10-CM 2025 guidelines emphasize using site-specific codes in addition to primary pain codes (such as G89.4 or G89.29) to capture the full clinical picture.
This section serves as a quick reference for coding chronic pain, acute pain, and pain not elsewhere classified, based on anatomical location and the presence of neurological or procedural complications.
Pain by Site: ICD-10-CM Code Reference
Practical Coding Tips
- Always pair G89.x codes with relevant site-specific diagnosis codes unless documentation clearly identifies pain as generalized.
- Document laterality (left, right, bilateral) when applicable to avoid non-specific codes.
- For implants or prosthetic devices, note any complications, follow-up visits, or pain control failures.
- Pain by site should also include the underlying cause (e.g., injury, surgery, trauma, neoplasm) to support medical necessity.
Site-Specific Pain and Psychological Factors
When pain affects functional or emotional well-being, or arises exclusively from psychological factors, additional coding is necessary. Pair physical site codes with:
- F45.41 – Pain disorder with both psychological and physical factors
- F45.42 – Pain disorder exclusively related to psychological factors
- G89.4 – Chronic pain syndrome (when psychosocial dysfunction is present)
Properly assigning ICD-10-CM diagnosis codes for pain that is localized, related to the nervous system, or chronic not elsewhere classified, ensures that treatment decisions and reimbursement outcomes are aligned with regulatory expectations.

Behavioral and Psychological Factors Affecting Chronic Pain
Chronic pain is rarely confined to physical symptoms alone. In many cases, especially those involving long-term musculoskeletal, neurological, or neoplasm-related pain, patients also experience emotional and behavioral complications. The 2025 updates to ICD-10-CM diagnosis codes reinforce the importance of coding related psychological factors when they contribute to or result from chronic pain disorders.
When to Code Psychological and Behavioral Factors
Use psychological and behavioral codes when:
- Pain is influenced or intensified by emotional or cognitive symptoms.
- The patient exhibits depression, anxiety, sleep disturbances, or psychosocial dysfunction.
- The pain is exclusively related to psychological factors, or is a mixed pain disorder.
- There is a need for neuropsychological or behavioral assessment as part of pain management.
These scenarios are particularly common in cases of:
- Chronic pain syndrome
- Complex regional pain syndrome
- Central pain syndrome
- Neoplasm-related pain (acute or chronic)
- Pain following traumatic injury or surgery
Key ICD-10-CM Codes for Psychological Factors in Pain

These codes are essential when pain disrupts mood, cognition, sleep, or behavior. The note instructs coders to use additional codes to indicate symptoms like insomnia, fatigue, or anxiety, especially when they complicate a primary diagnosis of chronic pain.

Behavioral Assessment Testing: When and How to Code
When evaluating psychological factors associated with chronic pain, healthcare professionals often use structured testing. These assessments help clarify how mental health status influences pain control, functioning, and treatment adherence.
CPT Codes for Assessment Services

These services are typically used in patients with:
- Diseases of the nervous system
- Chronic pain of uncertain origin
- Post-trauma symptoms
- Suspected somatization or pain amplification disorders
Documentation and Reimbursement Notes
- Document why the assessment is medically necessary (e.g., evaluating treatment barriers, ruling out malingering, assessing emotional distress).
- Link the testing to the patient’s pain-related diagnosis using the appropriate ICD-10-CM diagnosis code.
- Always verify payer-specific rules for behavioral health and neuropsychological testing, as pre-authorization is often required.
- Avoid using pain unspecified type codes when a psychological or neurobiological basis is documented.
Correctly coding for psychological factors associated with pain not only improves care coordination but also ensures appropriate reimbursement and compliance. As chronic pain management becomes more interdisciplinary, capturing the full scope of the condition, including emotional and behavioral consequences—becomes essential.
Documentation Must-Haves (Checklist)
Accurate documentation is the foundation of successful ICD-10-CM diagnosis code assignment for chronic pain and related disorders. With the expanded guidance in 2025, coders and providers must ensure that clinical records contain enough detail to justify the use of specific diagnosis codes, especially those addressing chronic pain syndrome, pain due to trauma, pain disorders exclusively related to psychological factors, and site-specific pain conditions.
Incomplete documentation can lead to the assignment of a billable non-specific code, such as “pain not elsewhere classified” or “pain NOS,” which may result in claim denials, audits, or underpayment. Below is a compliance-oriented checklist for clinicians and coding teams.

Chronic Pain Coding Documentation Checklist
Pain Characteristics
- Onset and duration: Indicate whether the pain is acute, chronic, or recurrent
- Specific timeframe: Document duration exceeding 3 months for chronic pain
- Type of pain: Include descriptors such as localized pain, generalized pain, or radiating pain
- Location: Identify the precise anatomical site (e.g., cervical region, thoracic region, lumbosacral region, upper limb, lower limb)
- Laterality: Specify left, right, or bilateral involvement
- Intensity: Include numerical pain scores or functional limitations caused by the pain
Underlying Cause and Course
- Identify any underlying condition (e.g., arthritis, cancer, surgery)
- Note if the initial injury is still contributing to pain or has resolved
- Confirm if the pain is now a diagnosis of its own (e.g., chronic pain syndrome)
Associated Symptoms and Complications
- Indicate presence of psychological factors such as depression, anxiety, insomnia, or fatigue
- Describe impact on activities of daily living (mobility, sleep, work, appetite)
- Note any neurological symptoms (e.g., numbness, tingling, weakness)
- List behavioral signs or emotional stress if applicable (supports coding of pain disorders exclusively related to psychological factors)
Treatment Plan and Functional Goals
- Specify pharmacologic interventions (e.g., nerve blocks, opioids, antidepressants)
- Document physical therapy, counseling, or referrals to pain specialists
- Record use of prosthetic devices, implants, or assistive technology
- Include details of patient education and pain control strategies
- Outline long-term management or surveillance plans
Special Circumstances
- Note complications such as chronic postprocedural pain or chronic post thoracotomy pain
- Clarify when pain is linked to external causes, such as accidents or surgical trauma
- Indicate whether pain is related to neoplasm (cancer) and whether it is acute or chronic
- Provide evidence supporting functional capacity evaluations or behavioral testing
By capturing these elements in the medical record, healthcare providers ensure they are using the most accurate type code to pain, whether it’s chronic pain not elsewhere classified, complex regional pain syndrome, or central pain syndrome. Doing so improves clinical communication, reduces denied claims, and supports a complete picture of the patient’s condition.
Action Steps for 2025 Readiness
With the 2025 ICD-10-CM diagnosis code updates introducing greater specificity for chronic pain, pain disorders, and psychological factors associated with pain, healthcare professionals must proactively adjust their clinical workflows, documentation protocols, and coding systems. These action steps are essential for ensuring accurate claims, avoiding denials, and delivering comprehensive chronic pain management.
This section outlines a practical roadmap for clinics, practices, and billing teams to become fully compliant with 2025’s coding expectations.

1. Conduct a Pain Coding Audit
- Review current use of G89.x, F45.x, and site-specific M- and G- series codes.
- Identify any overuse of non-specific codes (e.g., pain NOS, pain not elsewhere classified).
- Evaluate whether documentation consistently includes laterality, chronicity, and underlying conditions.
- Audit use of behavioral health codes related to chronic pain syndrome, neoplasm related pain, and central pain syndrome.
2. Update Clinical Documentation Templates
- Embed required elements into your EHR: pain duration, type (acute vs. chronic), body region, related psychological factors, and external causes.
- Add structured fields for documenting:
- Localized pain unspecified type
- Pain related to implants or prosthetic devices
- History of initial injury or postprocedural pain
- Ensure templates guide providers toward capturing functional impact and treatment response.
3. Train Your Clinical and Coding Teams
- Host team workshops or partner with certified coding specialists to review:
- Differences between billable specific code and billable non-specific code
- When to use pain disorders exclusively related to psychological factors
- Proper sequencing of primary diagnosis and secondary conditions
- Educate staff on how to identify qualifying conditions for:
- Complex regional pain syndrome
- Chronic post thoracotomy pain
- Neoplasm related pain acute or chronic
4. Automate Cross-Checking in Your Billing Software
- Leverage technology to:
- Flag mismatches between diagnosis and documentation (e.g., chronic pain coded without 3-month duration)
- Alert for missing related pain acute chronic indicators
- Batch verify pain control treatment plans against payer policies
- Integrate behavioral and physical codes for holistic pain management billing
5. Coordinate Pre-Authorization for Psychological and Functional Assessments
- Verify payer requirements for:
- 96132/96133 – Neuropsychological testing
- 96160 – Risk assessment instruments
- 95921 – Autonomic function testing
- Document how these evaluations relate to pain control, treatment planning, or symptom assessment
6. Monitor Changes to ICD-10-CM Quarterly
- Stay current with quarterly CMS updates, especially revisions involving:
- Diseases of the nervous system
- Causalgia and limb syndrome with pain
- Newly added subcategories for acute, chronic, or unspecified type pain
- Subscribe to coding bulletins that highlight changes for the upcoming fiscal cycle
7. Establish a Feedback Loop with Providers
- Share frequent denial patterns related to:
- Use of outdated or unspecified type codes
- Incomplete documentation of psychological factors
- Lack of specificity for upper limb or lower limb coding
- Encourage cross-disciplinary dialogue among physicians, therapists, coders, and billing teams
Taking these steps prepares your practice to meet 2025’s compliance standards, while improving reimbursement accuracy and supporting whole-person care for patients dealing with complex chronic pain conditions.
.avif)
Frequently Asked Questions
What are the key updates in ICD-10-CM changes for 2025 in chronic pain management?
The key updates for ICD-10-CM changes in 2025 regarding chronic pain management entail the introduction of new codes for chronic pain syndrome, specific site pain codes, and the incorporation of psychological factors in treatment. These changes aim to enhance the specificity and comprehensiveness of chronic pain documentation.
Why is accurate coding important for chronic pain management?
Accurate coding is crucial for chronic pain management as it facilitates appropriate reimbursement, reduces the likelihood of insurance claim denials, and ensures precise patient records, all of which are vital for delivering effective patient care.
What is the significance of the G89.4 code in chronic pain management?
The G89.4 code is crucial in chronic pain management as it documents chronic pain syndrome and highlights significant psychosocial dysfunction, thereby guiding tailored treatment strategies.
How do site-specific pain codes improve chronic pain management?
Site-specific pain codes enhance chronic pain management by offering precise documentation of the patient's condition, which enables targeted treatments and improves overall patient outcomes. This accuracy also aids in optimizing reimbursement processes.
What tools can healthcare providers use for efficient chronic pain management coding?
Healthcare providers can enhance chronic pain management coding efficiency by utilizing EHR systems with integrated billing software, practice management software, and automated billing tools. These tools significantly improve coding accuracy and streamline practice operations.
References: